A game-changing approach to whole-person care and health plan outcomes

With healthcare costs continually rising and margins under increasing pressure, health plans are searching for smarter ways to manage costs for their business while optimizing outcomes for their members. The solution? Innovative health plans use smart technology to enable whole-person care – an integrated care delivery approach that combines physical, behavioral, and social healthcare to improve member experiences, clinical outcomes, and financial sustainability for health plans.
Here’s the challenge: Traditional, episodic healthcare models fail to deeply integrate physical and behavioral health, which can lead to higher costs, fragmented experiences, and poor long-term outcomes. This is especially true for individuals with chronic conditions:
-
One in four people with a chronic condition also has a mental health disorder, yet they often receive treatment in separate, disconnected settings.
-
The cost of care for individuals with both behavioral and medical conditions can be 2-3Xs higher than for individuals with only medical illness.
-
Health plans and employer groups bear the cost burden of unnecessary hospitalizations, ER visits, and nonadherence to treatment plans.
Where’s the failure point in traditional approaches? Most third-party condition management technology applications are siloed. These programs deliver high-quality specialty care but are disconnected from the perspectives of care delivery, member experience, and data collection teams and are costly to manage separately.
This begs the question: What if health plans didn’t have to choose between prioritizing cost savings OR better outcomes – but could have both?
What does whole-person care mean? Partnering for success.
The average health plan has more than nine point solutions, leading to fragmented care delivery and experiences for members and increased total cost of ownership for the business. That leads to:
-
Lack of care coordination: Members and care teams struggling to navigate disjointed programs and members facing barriers to understanding what programs they’re eligible for.
-
Operational inefficiencies and sneaky costs: Clunky and time-consuming management of multiple vendors, contracts, billing needs, and workflows along with health plans missing out on cost savings from bundled opportunities.
-
Implementation and security complexity: Multiple rollout timelines and support teams, disparate datasets, and misaligned and complicated processes.
The Amwell approach solves these challenges so your team can deliver better care and more connected offerings with less time and resource investment.
We provide whole-person care for health plans and members by integrating virtual primary care, digital behavioral health, and a comprehensive set of condition-specific programs into a single platform and connected experience.
5 best practices to create an outstanding whole-person care program:
-
Single, connected experience: Create an easy-to-enter white-label digital front door that aligns with your company’s trusted brand. Seamless navigation across programs and access to all kinds of care in a cohesive environment eliminates confusion and ensures a frictionless healthcare journey.
-
Personalized and longitudinal care: Deliver a dashboard view where members only see programs included in their covered benefits and can intuitively self-enroll in clinical programs that meet their needs. A personalized experience that empowers members to manage their health long-term can make a difference in their satisfaction and engagement levels.
-
Intelligent referral management: A model that enables clinician-driven referrals, ensuring members receive timely and clinically appropriate care, can reduce gaps in care, enhance adherence to treatment plans, and ultimately improve clinical outcomes.
-
Unified data and insights: Integrate real-time analytics across all programs to enable health plans to track engagement, measure impact, and optimize cost savings. Unified data gives health plans a complete, longitudinal view of member health and program effectiveness.
-
Administrative ease: Establish simplified program management via one platform with integrated support across all point solutions and clinical partner programs. This can help health plans reduce operational complexity, enhance security and oversight, and streamline vendor management.
This is what Amwell does best – we help health plans establish a transformational whole-person care program.
Powering whole-person care through integrated virtual and digital care solutions
At Amwell, we help health plans transform whole-person care by integrating virtual primary care, digital behavioral health, and best-in-class condition-specific programs from third-party applications via the Amwell platform.
We offer much more than a “digital front door”; this environment expands the depth and breadth of what you can offer to members.
Discover Amwell’s whole-person care approach and impact on health plan outcomes
Amwell clinical partner programs
Health plans can partner with Amwell to offer members a growing set of Digital First® clinical partner programs to receive condition-specific, high-quality care with measurable impact:
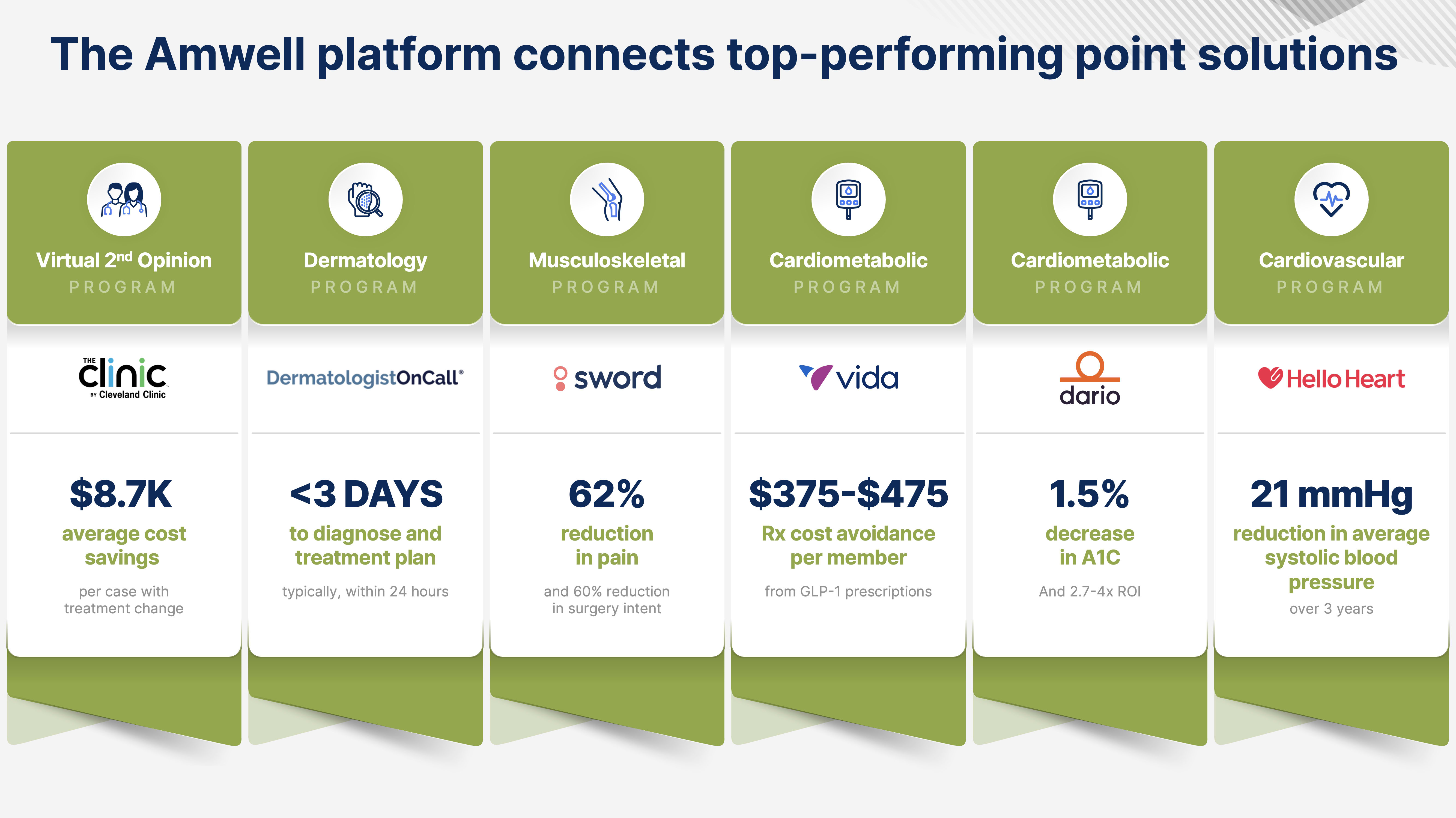
By seamlessly weaving these proven programs into your existing offerings, health plans can cut costs and keep members healthy, happy, and in-network.
See all Amwell clinical partner programs
Ready to see how Amwell can transform your approach to whole-person care?